Reducing Denials, Restoring Revenue
Targeted Denial Management Services for Healthcare Providers
At MediFunding Consulting, we help clinics, provider offices and private practices tackle claim denials with precision and strategy. Our denial management services are designed to identify the root causes of claim failures, recover lost revenue, and prevent future issues. From reworking denied claims to implementing long-term process improvements, we simplify the complex world of denial management in medical billing so you can focus on delivering quality patient care.
Expert Denial Management Healthcare Solutions
Claim denials don’t just delay payments—they drain resources and impact care delivery. At MediFunding Consulting, we offer expert denial management healthcare solutions that go beyond resubmission. We analyze denial trends, fix underlying issues, and create a proactive strategy to minimize future denials. Whether it’s a coding error, missing documentation or payer-specific requirements, we’ve seen it and solved it.
As a trusted partner in claim denial management services, we help you accelerate cash flow, improve claim success rates and reduce administrative burden.
Why Denial Management Matters More Than Ever
- Missed deadlines and lost reimbursements
- Compliance risks and coding disputes
- Increased operational overhead
- Reduced cash flow predictability
- Improve clean claim rates
- Reduce recurring rejections
- Strengthen payer relationships
- Focus more on patient care and less on paperwork
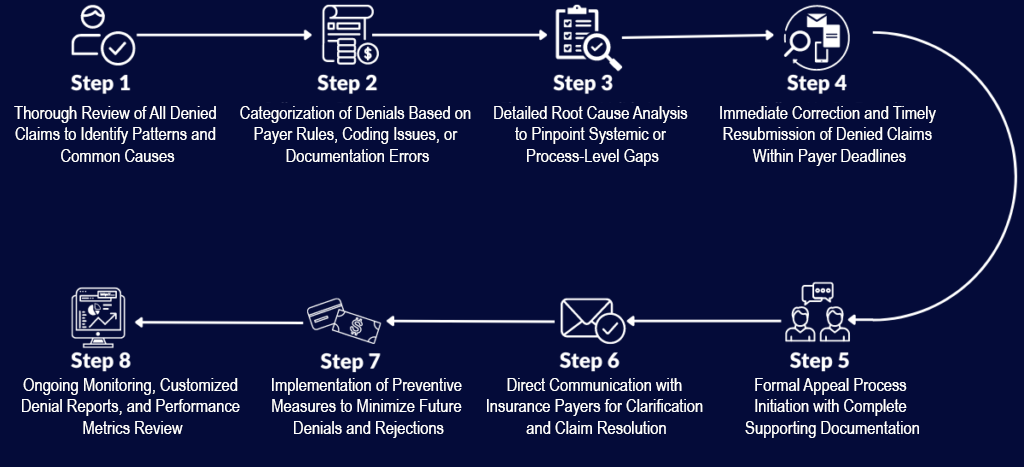
Our Optimized Denial Management Workflow
Denial Identification & Categorization
We review all denied claims and categorize them by root cause, payer, and claim type for targeted resolution.
Root Cause Analysis
In-depth analysis of patterns and processes leading to denials—so we can eliminate recurring issues at the source.
Corrective Action & Resubmission
Our specialists correct and resubmit denied claims quickly to maximize recovery within payer deadlines.
Appeal Management
We handle formal appeals with complete documentation, ensuring compliance with each payer’s requirements.
Payer Communication & Follow-Up
We directly liaise with payers to resolve disputes and ensure timely responses and payments.
Denial Prevention Strategy
Using real-time denial data, we refine your front-end processes to stop denials before they occur.
Compliance Review
We ensure all resubmitted and appealed claims meet regulatory and contractual requirements.
Custom Denial Reporting
You get clear, actionable reports on denial trends, recovery rates, and improvement areas.
Why Choose MediFunding?
Denial-Focused Expertise
Unlike general billing firms, we specialize in denial management healthcare, ensuring nothing slips through the cracks.
Payer-Specific Knowledge
Our team understands the nuances of payer rules and appeal processes to get faster results.
Recovery-Driven Approach
We don’t just resubmit—we fight for every dollar you're owed through expert appeal strategies.
Root Cause Elimination
We help your team prevent repeat denials by fixing upstream issues across documentation, coding, and billing.
Real-Time Insights
Access clear denial dashboards and custom reports that inform smarter financial decisions.
Flexible Integration
Our services easily integrate with your existing EHR and billing systems for a seamless workflow.
Complete Denial Management and Recovery
Our tailored claim denial management services give you control over revenue loss and the tools to prevent it. From high-volume hospital claims to specialty practices, we offer full visibility, faster recoveries, and fewer denials.
Additional Denial Support Services

Denials Trend Analysis & Prevention Strategy
Uncover patterns in payer rejections and implement fixes that stick.

Appeals Submission & Tracking
Expert handling of all appeals with documentation and timely follow-up.

Insurance Verification & Authorization Review
Audit and refine front-end processes to catch issues before claims are submitted.

Clinical Documentation Review
Ensure provider notes fully support medical necessity and accurate coding.

Payer Contract Review
Evaluate your payer agreements to identify underpayments and enforce proper reimbursements.

Back Office Denial Support
Let our denial experts manage the follow-up, reporting, and appeals—freeing up your team’s time.
Types of Claim Denials
Understanding the types of claim denials is key to effectively managing and reducing them.
Hard Denials
Hard denials are irreversible and lead to permanent revenue loss, typically caused by compliance issues or missed deadlines, and are rarely eligible for appeal.
Soft Denials
Soft denials are temporary and reversible, often due to missing information, coding mistakes, or billing discrepancies, and can be corrected with timely follow-up.
Preventable Denials
Preventable denials occur due to avoidable errors like incorrect coding or late submissions and highlight the need for better training and quality control.
Clinical Denials
Clinical denials stem from questions around medical necessity or care levels and are difficult to appeal due to strict payer guidelines and documentation requirements.
Administrative Denials
Administrative denials are usually soft and result from technical issues like incomplete patient information, easily resolved by updating records and resubmitting the claim.
Ready to Take Control of Denials?
Partner with MediFunding Consulting, your trusted ally in denial management healthcare.
Our expert team helps reduce write-offs, recover missed revenue and build denial-resistant processes that strengthen your financial health. Are you a hospital? Multi-specialty clinic? Or solo practice? We’re here to help YOU.
Contact us today for a free consultation and discover how focused denial management in medical billing can transform your revenue cycle.
